Overview
Obsessive-Compulsive Disorder (OCD) is recognized as a disability under the Americans with Disabilities Act (ADA). This acknowledgment is crucial because OCD significantly impacts major life activities, including work and social interactions. We understand that living with OCD can be incredibly challenging, hindering daily functioning and affecting relationships.
It's essential to know that there are legal criteria in place for obtaining support and accommodations. This support can make a meaningful difference in your life. Emphasizing the importance of treatment and advocacy, we encourage those affected to seek help. Remember, you are not alone in this journey, and there are resources available to assist you.
Introduction
Obsessive-Compulsive Disorder (OCD) is more than just an anxiety condition; it profoundly disrupts daily life. This raises critical questions about its recognition as a disability. We understand that navigating this reality can be overwhelming. Understanding the legal framework surrounding OCD is essential. It not only impacts the lives of those affected but also opens doors to necessary support and accommodations in various settings.
Yet, despite the availability of treatment options and legal protections, many individuals grapple with misconceptions and stigma. These barriers can hinder their pursuit of help. It's common to feel isolated in these struggles. How does society reconcile the challenges posed by OCD with the rights and resources available to those who live with it? Together, we can work towards a better understanding and support for everyone affected.
Define Obsessive-Compulsive Disorder (OCD)
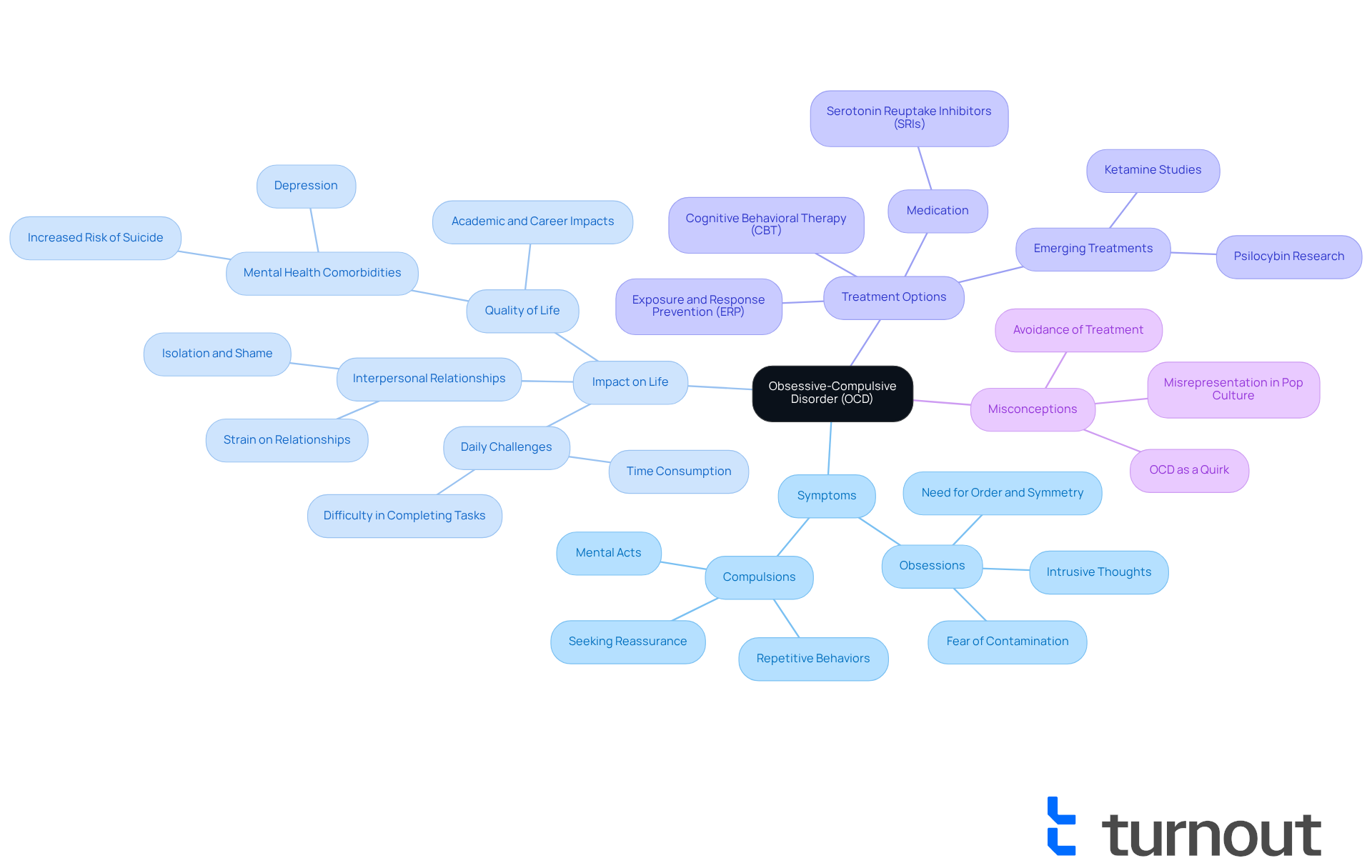
Obsessive-Compulsive Disorder (OCD) is a complex mental health condition that can be incredibly challenging. It is characterized by persistent, intrusive thoughts known as obsessions, which are often accompanied by repetitive behaviors or mental acts called compulsions. Many individuals with OCD feel an overwhelming urge to perform these compulsions to ease the anxiety triggered by their obsessions or to prevent a feared outcome. Common fears include contamination, harm, or an overwhelming need for order and symmetry.
We understand that the impact of OCD on daily life can be profound, leading many to ask, is OCD a disability? Research shows that untreated OCD raises the question of is OCD a disability, as it can consume an entire day and lead to significant challenges in interpersonal relationships, social interactions, and work. Fortunately, approximately 70% of people with OCD find relief through exposure and response prevention therapy (ERP) and/or medication. This highlights the treatability of the condition. However, misconceptions about OCD can lead to feelings of isolation and avoidance of treatment, even when help is available.
Real-world examples can shed light on the debilitating effects of OCD. Take Uma Chatterjee, for instance. She began experiencing symptoms at just four years old, facing immense challenges in her academic and social life due to her compulsive behaviors. Her story is a powerful reminder of the importance of effective treatment. Through ERP therapy, she found relief and was able to pursue a successful academic career in neuroscience, while also advocating for others with OCD. Uma poignantly notes, 'OCD is so misrepresented in pop culture,' which can complicate understanding and acceptance of this condition.
Comprehending the traits of OCD and its significant impact on quality of life is essential for recognizing if is OCD a disability that requires support. It’s also important to acknowledge the coexisting signs of depression and the heightened risk of suicide associated with OCD. This underscores the gravity of the condition and the necessity for those affected to seek the assistance they deserve. Remember, you are not alone in this journey, and help is available.
Explore OCD as a Recognized Disability
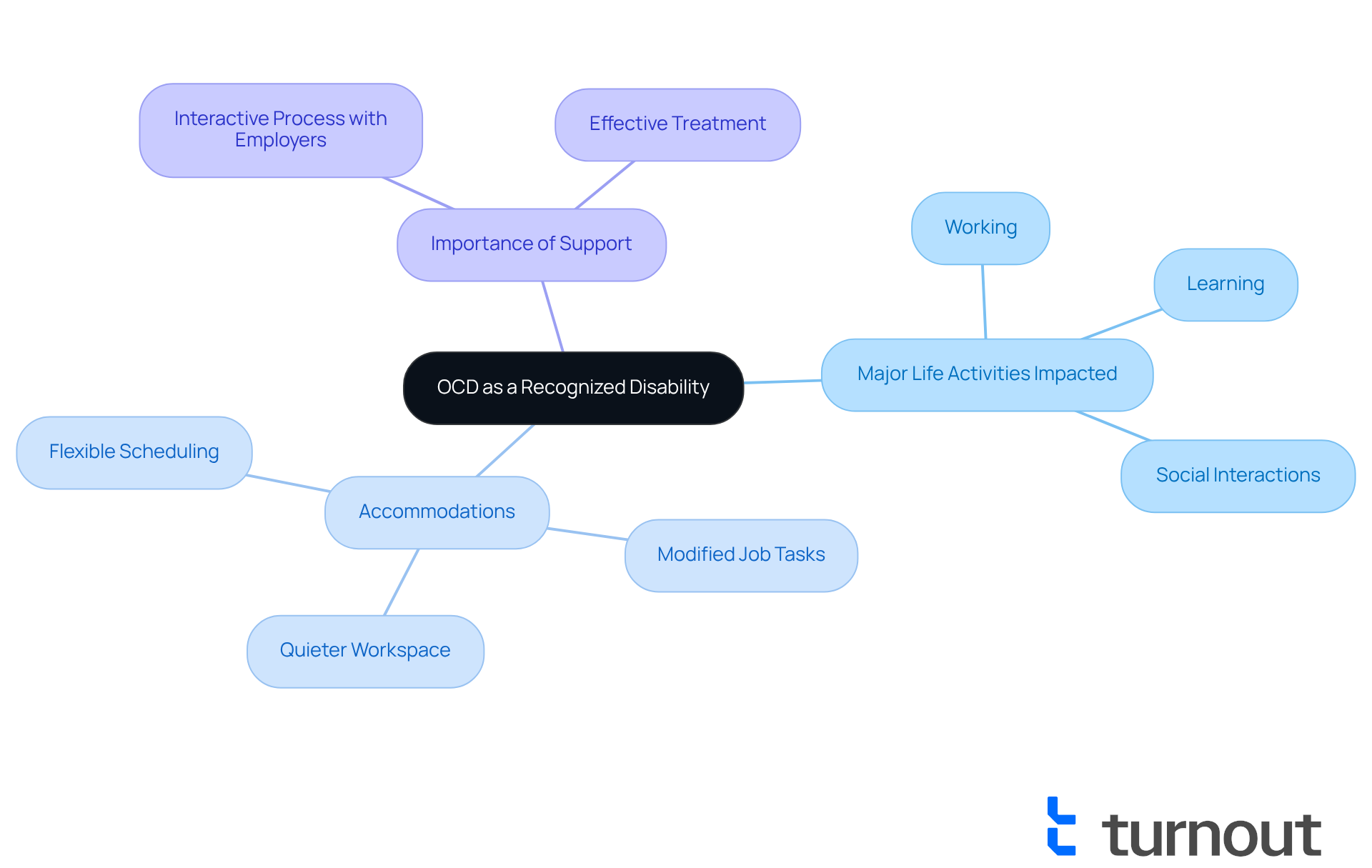
Obsessive-Compulsive Disorder (OCD) is a disability that is officially recognized under the Americans with Disabilities Act (ADA). This recognition is significant, as it can greatly limit one or more major life activities, such as working, learning, or social interactions, which leads to the discussion of whether OCD is a disability. We understand that living with OCD can be challenging, but this classification allows individuals to seek necessary adjustments in both professional and educational settings.
For instance, employees may request:
- Flexible scheduling
- Modified job tasks
- A quieter workspace
to better manage their symptoms. Research indicates that approximately 60% of individuals with OCD actively seek suitable adjustments to enhance their job performance and overall well-being. It's common to feel overwhelmed, but supporters like Hussain Hussain emphasize the importance of these adjustments in fostering an inclusive workplace. As Hussain states, "With effective treatment, existence can become more manageable, fulfilling, and empowering."
As the conversation around workplace inclusivity grows, it's crucial for employers to engage in the interactive process. This collaboration helps identify reasonable accommodations, ensuring that individuals receive the resources they need to navigate daily challenges effectively. The impact of OCD on job performance can be profound, often leading to difficulties in concentration and productivity.
However, with effective treatment and support, many individuals can manage their OCD symptoms. This journey can lead to a more fulfilling and productive life. Remember, you are not alone in this journey, and we’re here to help you find the support you need.
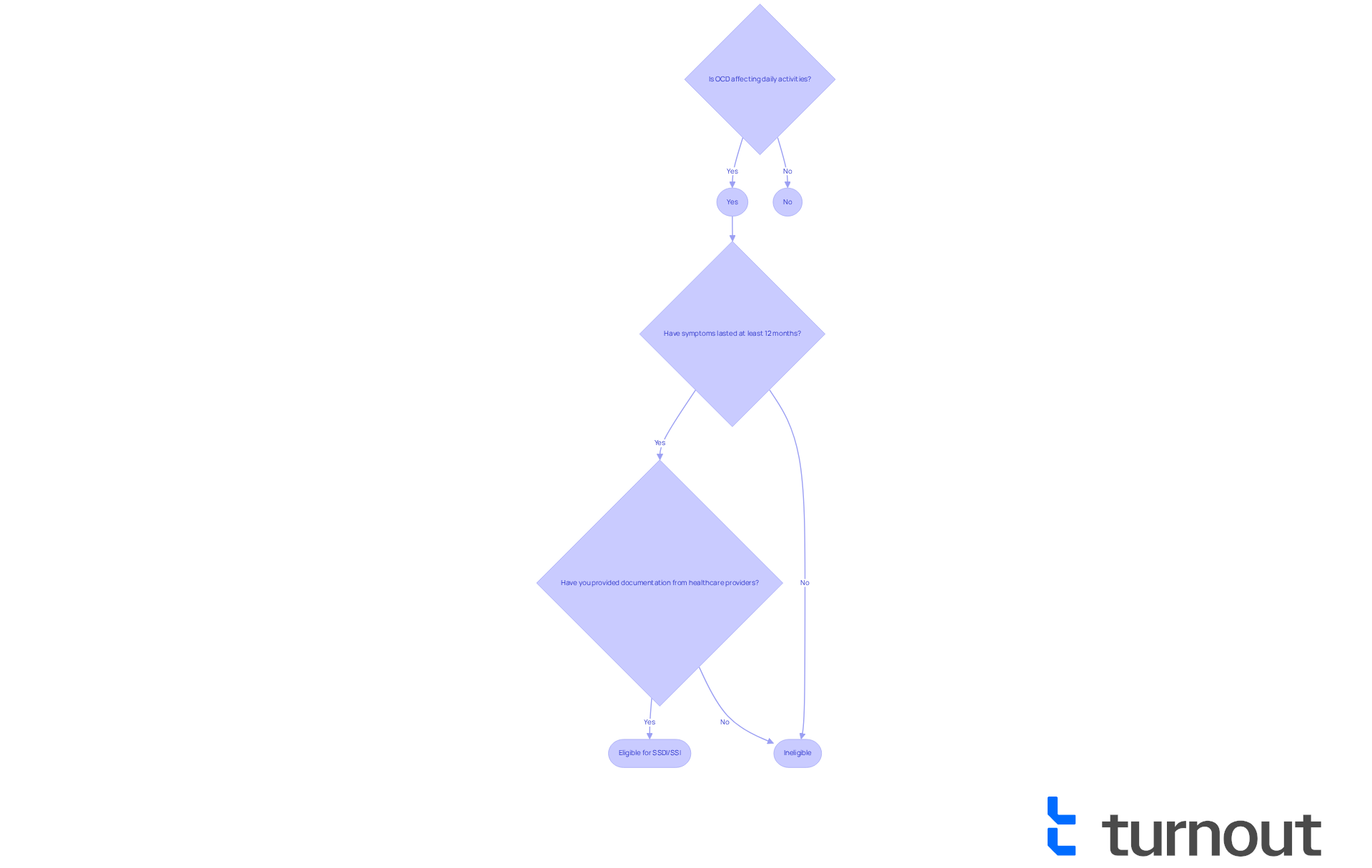
Understand Legal Criteria for OCD Disability Classification
We understand that living with Obsessive-Compulsive Disorder (OCD) can lead to discussions about whether OCD is a disability, especially when it affects your ability to perform daily activities. To qualify for disability benefits, it’s essential to demonstrate how your condition, including the question of whether OCD is a disability, significantly hinders your capacity to manage these essential tasks. The Social Security Administration (SSA) has outlined specific criteria, focusing on the severity and duration of your symptoms.
For instance, if your OCD symptoms prevent you from maintaining a job or carrying out daily activities for at least twelve months, it raises the question of whether OCD is a disability, which may make you eligible for Social Security Disability Insurance (SSDI) or Supplemental Security Income (SSI). It’s important to provide comprehensive documentation from your healthcare providers, detailing how OCD impacts your functioning. This documentation should include evidence of intrusive thoughts, compulsive behaviors, and the resulting limitations in your daily living activities, social interactions, and overall mental health.
Meeting these criteria is crucial for a successful claim. The SSA carefully assesses each case based on the question of whether OCD is a disability that affects your ability to engage in full-time work activities. Remember, you are not alone in this journey, and we’re here to help you navigate the process with care and understanding.
Examine Rights and Support for Individuals with OCD
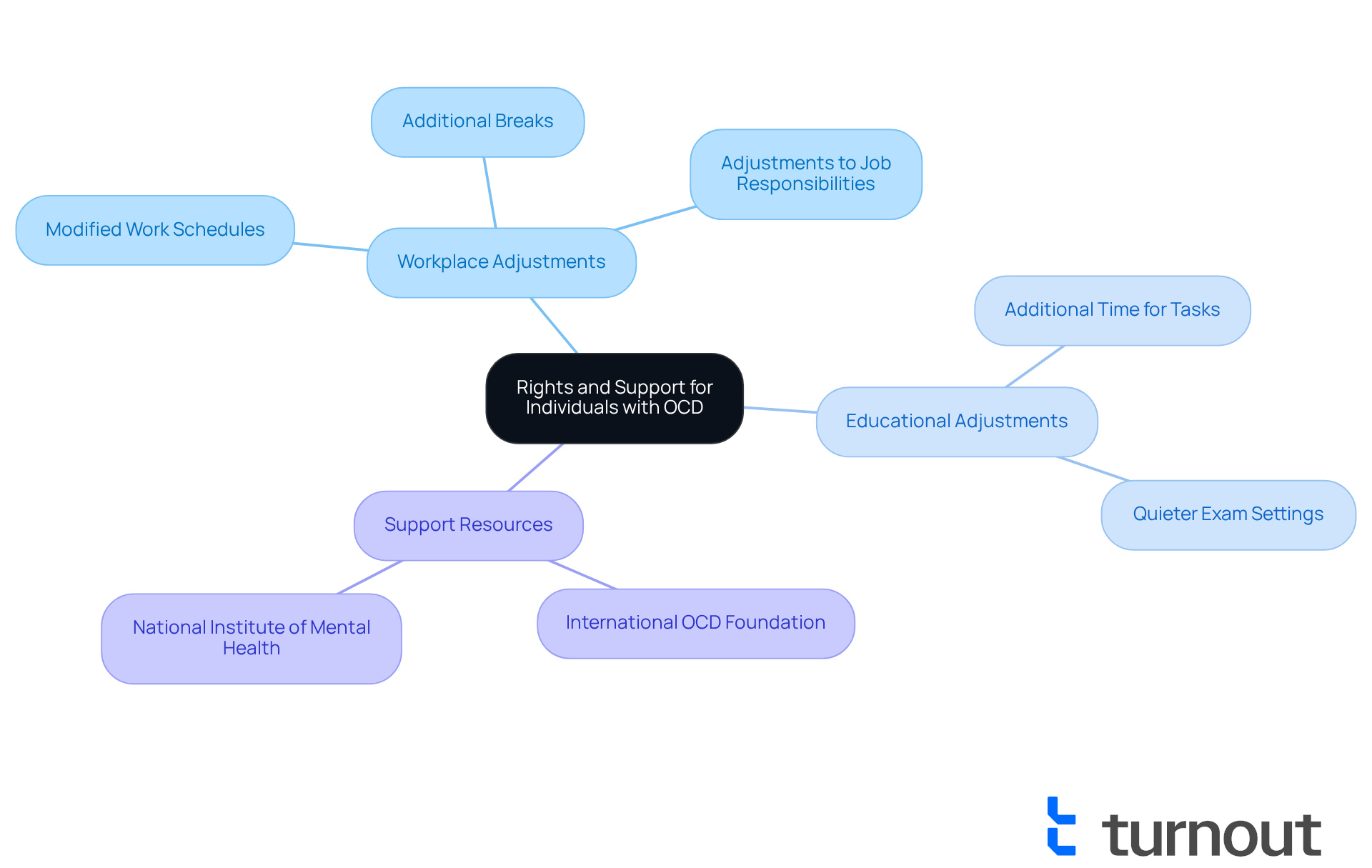
Individuals with OCD have specific rights under the Americans with Disabilities Act (ADA), which includes the opportunity to seek appropriate adjustments in both workplace and educational settings. These accommodations can take various forms, such as:
- Modified work schedules
- Additional breaks
- Adjustments to job responsibilities
Each of these adjustments aims to assist individuals in managing their symptoms effectively. It's important to recognize that approximately 18% of U.S. workers report having a mental health condition, highlighting the necessity for supportive measures in the workplace.
Support resources are essential for those managing OCD. Organizations like the International OCD Foundation offer valuable information and community support, connecting individuals with others who share similar experiences. Accessing these resources can significantly enhance the quality of life for those affected by OCD. For instance, the National Institute of Mental Health states, 'Is OCD a disability under certain conditions, particularly when it significantly impairs an individual’s ability to perform essential life activities?'
In educational environments, suitable adjustments may include:
- Additional time for tasks
- The option to take exams in a quieter setting
These changes can reduce stress and improve performance.
In workplaces, effective adjustments might involve:
- Flexible scheduling
- Designated quiet areas
- The use of project management tools to help organize tasks
These accommodations not only support those with OCD but also foster a more inclusive and productive atmosphere for everyone. By recognizing that OCD is a disability, individuals can advocate for necessary accommodations to navigate their challenges more effectively and lead fulfilling lives. Remember, you are not alone in this journey, and there are resources available to help you thrive.
Conclusion
Obsessive-Compulsive Disorder (OCD) is not just a mental health condition; it is a recognized disability that can significantly impede daily functioning. We understand that navigating this reality can be challenging. Understanding OCD's classification under the Americans with Disabilities Act (ADA) is crucial for individuals seeking support and accommodations. This recognition empowers you to advocate for your rights and access the necessary resources to manage your symptoms effectively.
This article highlights multiple facets of OCD, including its definition and the profound impact it can have on daily activities. Real-life narratives, like that of Uma Chatterjee, illustrate the challenges faced by individuals with OCD while emphasizing the importance of treatment and support. It’s common to feel overwhelmed, but it’s important to know that you have the right to seek reasonable accommodations in both educational and workplace settings. These adjustments can enhance your ability to thrive despite the challenges posed by the disorder.
Ultimately, recognizing OCD as a disability is a step towards fostering a more inclusive society. Together, we can create a supportive environment where individuals with OCD receive the help they need, whether through workplace adjustments or access to mental health resources. By promoting awareness and understanding, we can help dismantle the stigma surrounding OCD. Remember, you are not alone in this journey; we encourage you to seek help, advocate for your rights, and lead a fulfilling life.
Frequently Asked Questions
What is Obsessive-Compulsive Disorder (OCD)?
Obsessive-Compulsive Disorder (OCD) is a complex mental health condition characterized by persistent, intrusive thoughts known as obsessions, which are often accompanied by repetitive behaviors or mental acts called compulsions. Individuals with OCD feel an overwhelming urge to perform these compulsions to alleviate anxiety triggered by their obsessions.
What are common fears associated with OCD?
Common fears associated with OCD include contamination, harm, and an overwhelming need for order and symmetry.
Can OCD be considered a disability?
Research indicates that untreated OCD can significantly impact daily life, interpersonal relationships, and work, leading to the question of whether it is a disability. Its debilitating effects can consume an entire day, highlighting the need for support.
How effective is treatment for OCD?
Approximately 70% of people with OCD find relief through exposure and response prevention therapy (ERP) and/or medication, indicating that the condition is treatable.
What are the consequences of misconceptions about OCD?
Misconceptions about OCD can lead to feelings of isolation and avoidance of treatment, even when help is available, complicating understanding and acceptance of the condition.
Can you provide an example of someone affected by OCD?
Uma Chatterjee experienced OCD symptoms from the age of four, which impacted her academic and social life. Through ERP therapy, she found relief and was able to pursue a successful career in neuroscience while advocating for others with OCD.
What should be acknowledged regarding coexisting conditions with OCD?
It is important to recognize the coexisting signs of depression and the heightened risk of suicide associated with OCD, emphasizing the necessity for those affected to seek the assistance they deserve.



